Authors: Baris Kocaoglu, Julio Calleja-González, Igor Jukic, Francesco Cuzzolin, Mar Rovira, Antonio Santo, Jaime Sampaio
Basketball carries the risk of developing overuse injuries, which in the bone consist of bone stress injury (BSIs) or bone marrow edema (BME). The BSI occurs when a bone cannot withstand repetitive mechanical loading, resulting in structural fatigue, localized bone pain and tenderness. BSIs are a pathological process that begins with stress reactions and can progress to stress fractures and ultimately complete bone fractures. When BME happens, it sometimes takes 2 months for a player to return to play, which makes it of the most challenging injuries in EuroLeague.
Identifying contributing risk factors and developing appropriate management strategies when it occurs, is essential to prevent BSI in basketball players. Considering its microdamage-centered pathophysiology, it is conceivable that BSI mostly occurs when the mechanical stimulus at a particular bone site is above the threshold of microdamage formation. Risk factors for BSI can be grouped into two categories: factors modifying the load applied to a bone and the ability of a bone to resist load without damage accumulation (1). Factors modifying the load applied to bone include biomechanical factors, training factors, muscle strength and endurance, training surface, and terrain, shoes & inserts (insoles). Factors modifying the ability of a bone to resist the load include: genetics, diet and nutrition, endocrine status and hormones, physical activity history, bone diseases and medications influencing the bone.
It is difficult to make a clinical diagnosis of BSI at its beginning. They usually present as overuse injuries. An astute clinician can diagnose pathology at the stress reaction stage; however, some players may not present it until the pathology has progressed to a stress fracture with actual cortical disruption. A thorough history is the first step in diagnosing BSI. In most cases, individuals with BSI have a history of pain. Because initial pain usually subsides immediately after practice is completed and doesn’t occur during rest, it is often ignored at first (2). However, with continued training and progression of pathology, pain may become more severe, localized and occur at an earlier stage of the training. It may also persist longer after running is completed and may begin to occur during activities that involve lower levels of bone load, such as walking. Eventually, pain may lead to restriction of running and jumping or to the need to stop training. In more advanced stages, it may cause pain during rest and at night. The most distinctive feature of BSI during physical examination is localized bony tenderness. Basketball players who show clinical sign and symptoms of a possible BSI need imaging to make a definitive diagnosis. Of the imaging methods currently available, magnetic resonance imaging is the method of choice due to its superior contrast resolution (3).
The high recurrence rate of BSIs suggests that the primary goal for team doctors when managing low-risk BSIs should be to identify and modify potential risk factors for future BSIs. Using the concept that BSIs occur when the applied load exceeds the bone’s ability to resist the load without accumulation of microdamage, basketball players with BSIs require strategies to reduce the applied load and increase the load bearing capacity of their skeleton.
In the early stages of BSI management, the goal of treatment is to be pain free during and after normal activities of daily living. Walking should be minimized and restricted to a normal walking pattern until necessary to perform activities of daily living. If a pain-free, normal walking pattern cannot be achieved, a short period with a walking boot or of non-weight bearing may be considered. However, in all scenarios, one should try to progress to unaided, pain-free walking as soon as possible. During this period, it is essential to identify potential risk factors that contribute to the formation of BSI and to remove these factors from the player. Besides, load management and strength training are very important in maintaining proper neuromuscular activation, thereby reducing joint and skeletal overloading.
Maintaining load management and strength training during recovery after BME, to the extent permitted by the athlete’s pathology, is important for return to sport. Since athlete’s experience decreases in cardiovascular performance after as little as 2 weeks, conditioning activities should be started early (4). There are multiple methods of maintaining cardiovascular fitness during recovery from a BSI, including cycling, swimming, deep water running and antigravity treadmill (Alter-G) training. When available, an antigravity treadmill may be utilized to replace over-ground running. This approach could enable an athlete to engage in running at higher intensities earlier in the recovery process, while minimizing the loading on the affected bone. As a result, activity modification can serve as a valuable tool for maintaining fitness levels while safeguarding the healing BSI site. During activity modification period, the role of strength training in maintaining proper neuromuscular activation is very important which will also help reducing joint and skeletal overloading.
Shoe inserts which are offloading the affected area are very helpful as both conservative treatment and protective after invasive treatment. If the player has medial femoral condyle or tibial plateau BME, 5-10 degrees lateral wedge shoe insert is very effective to shift the loading of the mechanical axis to unfaceted area. Concurrently, medial wedge inserts are very useful for lateral femoral condyle or tibial plateau BME.
Other factor, which has a vital importance, is proper athlete’s nutrition during bone edema treatment (e.g. Potential renal acid load (PRAL) negative and calcium rich), which fuels the athlete while reducing the intake of acid-forming foods. This helps mitigate bone demineralization caused by the production of organic acids during practices and competitions. Most plant proteins (such as lentils, beans and nuts) have a negative PRAL value, representing that these foods produce base in our body. To lower the PRAL of players diet, it is important to focus on consuming more base-forming foods, such as fruits, vegetables, and legumes, and reducing the intake of acid-forming foods, such as meats, cheeses, and processed foods. In case of BME, vitamin D supplementation is also very important. It is recommended to keep Vitamin D blood levels between 50 ng/mL and 100 ng/mL. It is always suggested to have vitamin D blood levels over 30 ng/mL to improve health status and over 50 ng/mL for athletic performance. We have to keep in mind that Vitamin D blood levels over 100 ng/mL would be harmful for liver cells, which are the main storage for the vitamin.
While there are currently no proven methods for expediting BSI-BME healing when conservative treatment is unsuccessful, several approaches have been proposed and are under consideration to decrease return to play time. These are;
- Low-intensity pulsed ultrasound therapy
- PRP or BMAC injection into the bone edema area
- Calcium phosphate injection into the bone edema area
- IV zoledronic acid and Alendronate injection therapy
One such method that shows promise is low-intensity pulsed ultrasound therapy. This treatment has garnered significant support due to its observed positive effects on the healing of complete bone fractures. Studies have shown that low-intensity pulsed ultrasound therapy has been effective in stimulating union in 98% of BSIs, while 94% of BSIs delayed union and non-union, respectively(5). Another treatment method used for BME is PRP or BMAC injection into the effected bone area. Although its effectiveness is debated in studies, some studies have shown better clinical results and short return to play time, like 2 or 3 weeks (6). Calcium phosphate injection into the bone is also among the treatment options. Limited data from the published studies would suggest that calcium phosphate injection of BME may potentially improve pain and function with short return to play time (7). However, no evidence is currently available to clearly identify patient/surgical factors that may influence the long-term outcomes of this procedure. Another treatment that can be applied to basketball players during the season for bone edema is IV Zoledronic acid and Alendronate injection therapy (Figure 1). Literature shows that during a season, the combination of therapies causes early pain relief and reduction of the bone edema, which becomes effective due to the importance of short return to play time (8).
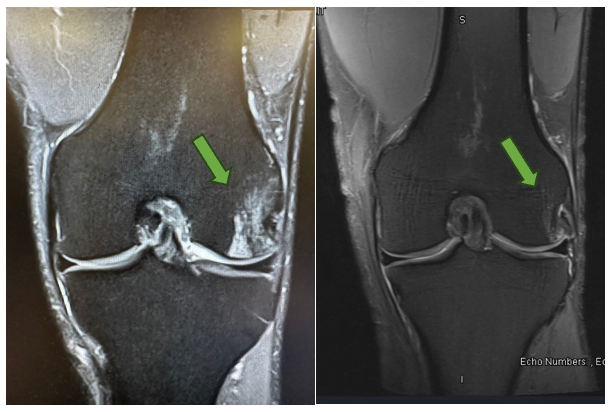
Figure 1: EuroLeague and national team player who was treated with IV zoledronic acid for BME during season. There was a significant improvement shown with MRI at three weeks period after treatment.
Overall, a comprehensive approach that addresses the underlying factor contributing to BSI development and that incorporates appropriate management strategies, is key to optimizing the health and performance of basketball players. A combination of defined therapies, including conservative treatment with activity modification, load management, strength training, modified shoe inserts and PRAL negative-calcium rich diet, could be used to provide quick return to play, which resembles our motto:
‘Keep the player on the court’.
REFERENCES:
Bennell KL, Malcolm SA, Thomas SA, Reid SJ, Brukner PD, Ebeling PR, et al. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med [Internet]. 1996 [cited 2024 Mar 10];24(6):810–8. Available from: https://pubmed.ncbi.nlm.nih.gov/8947404/
Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med [Internet]. 2001 [cited 2024 Mar 10];29(1):100–11. Available from: https://pubmed.ncbi.nlm.nih.gov/11206247/
Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology [Internet]. 2005 May [cited 2024 Mar 6];235(2):553–61. Available from: https://pubmed.ncbi.nlm.nih.gov/15858094/
Coyle EF, Martin WH, Sinacore DR, Joyner MJ, Hagberg JM, Holloszy JO. Time course of loss of adaptations after stopping prolonged intense endurance training. J Appl Physiol Respir Environ Exerc Physiol [Internet]. 1984 [cited 2024 Mar 9];57(6):1857–64. Available from: https://pubmed.ncbi.nlm.nih.gov/6511559/
Mayr E, Frankel V, Rüter A. Ultrasound–an alternative healing method for nonunions? Arch Orthop Trauma Surg [Internet]. 2000 [cited 2024 Mar 10];120(1–2):1–8. Available from: https://pubmed.ncbi.nlm.nih.gov/10653095/
Lin W, Xie L, Zhou L, Zheng J, Zhai W, Lin D. Effects of platelet-rich plasma on subchondral bone marrow edema and biomarkers in synovial fluid of knee osteoarthritis. Knee [Internet]. 2023 Jun 1 [cited 2024 Mar 20];42:161–9. Available from: https://pubmed.ncbi.nlm.nih.gov/37001332/
Angadi DS, Edwards D, Melton JTK. Calcium phosphate injection of symptomatic bone marrow lesions of the knee: what is the current clinical evidence? Knee Surg Relat Res [Internet]. 2020 Dec 1 [cited 2024 Mar 20];32(1):1–8. Available from: https://kneesurgrelatres.biomedcentral.com/articles/10.1186/s43019-019-0013-3
Agarwala S, Sharoff L, Jagani N. Effect of Zoledronic Acid and Alendronate on Bone Edema and Pain in Spontaneous Osteonecrosis of the Knee: A New Paradigm in the Medical Management. Rev Bras Ortop (Sao Paulo) [Internet]. 2020 Oct 1 [cited 2024 Mar 20];55(5):543. Available from: /pmc/articles/PMC7575358/




